The Role of Protein in Insulin Resistance Symptoms and Treatment
The role of protein in insulin resistance treatment
If you’ve followed me for any amount of time, you know that what’s missing from those posts from fitness influencers you follow on TikTok, is nuance. That’s what I bring to the table.
You might have already read my articles about protein quality and the health effects of a vegan diet. And still, you've bought into vegan protein shakes, and have shelves loaded with protein-enriched cookies, bars, and cereals. You’re feeling pretty good about meeting those higher protein intake recommendations that saturate your social feed.
But I’m here to dig deeper into the role of protein in insulin resistance symptoms, and why getting your protein from those sources might be making your insulin resistance symptoms worse, contributing to weight gain and inflammation.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
insulin resistance causes and symptoms
the role of protein in insulin resistance treatment
why protein quality matters just as much as quantity
more ways to improve insulin sensitivity symptoms
what is insulin resistance?
The word metabolism often gets referred to as one’s ability or inability to lose weight. But the word metabolism actually refers to the conversion of one component into another.
With digestion, metabolism might refer to ingested food being broken down into nutrients your body can use. Or a chemical component of medication or a food additive might be manipulated by enzymes into a neutralized form and removed from the body.
For the sake of this discussion, we’ll be referring to metabolism in regard to glucose metabolism - the conversion of glucose (a molecular form of sugar) into energy or fat.
It’s important to understand that glucose comes from more than just sugar ingredients. Glucose comes from all carbohydrates, including grains, starches, and yes, sugar.
So, whether it’s potatoes, sweet potatoes, rice, bread, legumes, fruit, honey, or candy - it all turns into glucose.
And that glucose either gets metabolized into energy or fat. Insulin, a hormone produced by the pancreas, is required for the metabolism of glucose into energy.
Here’s how glucose metabolism works:
When you consume any kind of carbohydrate, be it starchy legumes, grains, or vegetables, sugars like honey, fruit, or cane sugar, even leafy greens contain carbohydrates - those carbohydrates are broken down into molecules called glucose.
Glucose molecules are transported into your bloodstream through the epithelial lining of the small intestine. The amount of glucose molecules in your bloodstream at any given time is referred to as your “blood sugar” or “blood glucose” level.
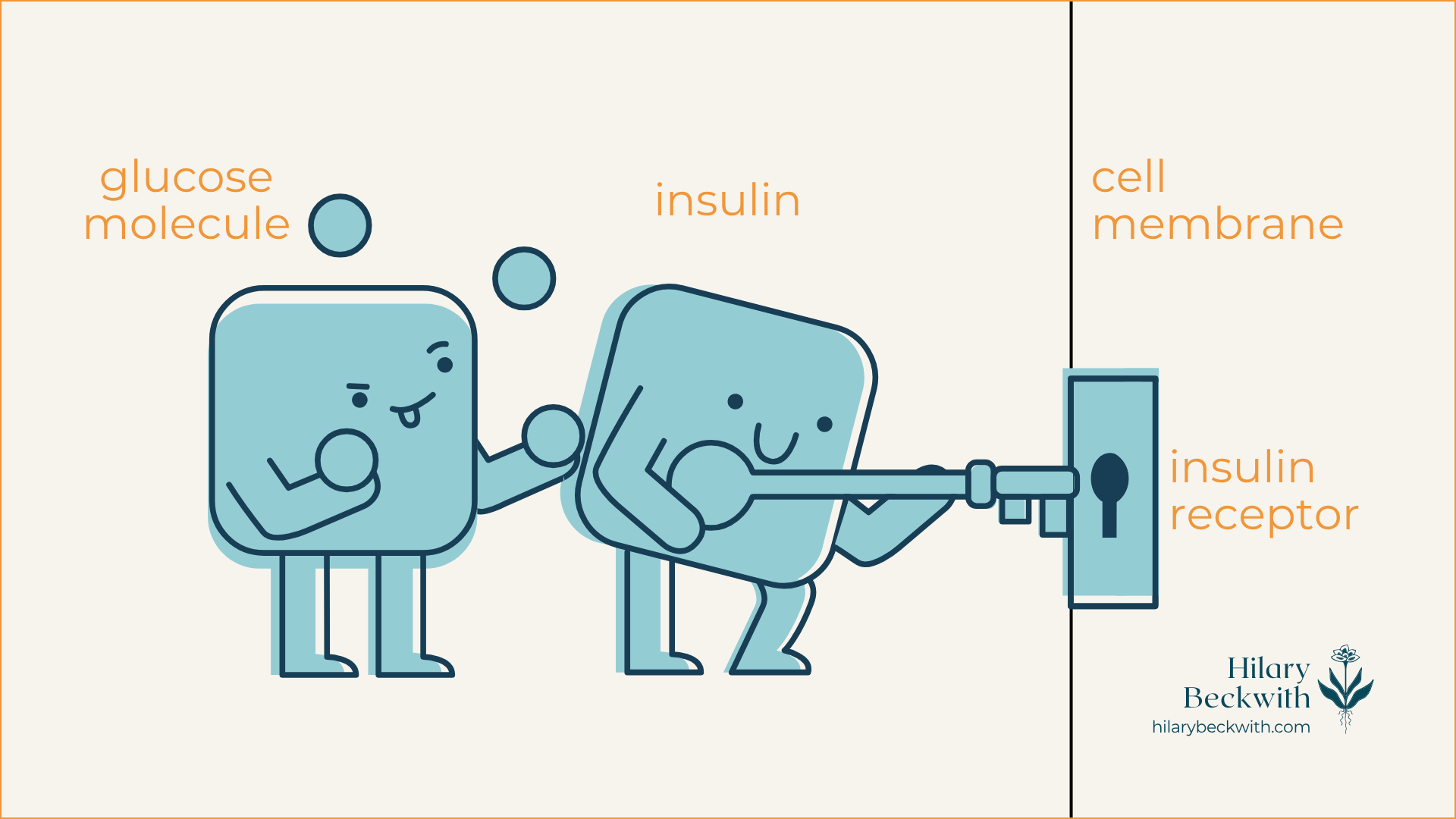
Insulin is released by the pancreas and acts as sort of an usher, taking the glucose to individual cells, and using its key to unlock the door (insulin receptors embedded in the cell membrane) and shuttles the glucose in to be metabolized (hey, there’s that word again!) via the Krebs cycle within the mitochondria.
When cells have had their fill of glucose, any glucose remaining is then sent to the liver and converted to storable forms of glucose, specifically glycogen and triglycerides.
Glycogen: stored primarily in the liver, and to some extent, muscles. The liver has a very small capacity for glycogen storage.
Triglycerides: stored as fat tissue, also called adipose tissue. Your body has unlimited stores of triglycerides in adipose tissue, as it can always (and does) make more fat to accommodate more triglyceride storage.
HERE’S WHERE THINGS CAN GO WRONG
Insulin resistance occurs when there is regularly more glucose than can be used by cells in the bloodstream. For example, one who consumes a high-carbohydrate diet at most meals and snacks will likely develop insulin resistance symptoms.
When there is regularly more glucose in the bloodstream than cells can accommodate, insulin receptors (remember the locked doors on cell membranes) begin to deactivate, making insulin ineffective. The cells are essentially saying, “we’ve had enough!”.
In response, the body produces more insulin to try and compensate for glucose not getting into cells, and as a result, insulin resistance worsens.
And what happens to glucose that does not enter cells? It gets converted to fat.
insulin resistance causes and symptoms
COMMON CAUSES OF INSULIN RESISTANCE
high starch, high carbohydrate diet
regular consumption of processed foods (including foods you might consider “health foods”, like protein powders, bars, shakes, and plant-based meat substitutes)
chronic stress (external or internal) - Click here to read more about the role of cortisol in blood sugar regulation
inactivity/sedentarianism
inadequate sleep
overexercising (especially cardio)
pancreatic insufficiency (more on what symptoms look like later in the article)
leaky gut syndrome
COMMON SYMPTOMS OF INSULIN RESISTANCE
weight gain in belly and/or hips
difficulty losing weight
“hangry” symptoms between meals (loss of focus, shaky, irritability)
digestive symptoms
pancreatic insufficiency can often contribute to digestive dysfunction, as it is needed to produce digestive enzymes
digestive symptoms are often indicative of pathogenic infection, such as yeast or bacterial overgrowth, mold, or parasites - all of which contribute to chronic stress response and cortisol output
excess hunger (frequent hunger, or excess appetite)
Type II Diabetes diagnosis, or pre-diabetes
abnormal thyroid labs (click here to read more)
sweet, salty, or carb cravings
the role of protein in insulin resistance treatment
It’s no secret that we need protein to build muscle - and that’s exactly the same reason it’s needed for insulin resistance treatment.
Let me explain.
HOW YOUR BODY BUILDS MUSCLES
A common misconception about building muscles, is that it requires an increase in the number of muscle cells (also called muscle fibers) - but this is incorrect. Your body actually cannot produce more muscle cells.
Muscle cells can, however, get larger in size - this is what is known as hypertrophy.
Additionally, contained in the fluid between muscle cells are smaller stem cells called satellite cells. In addition to hypertrophy, the satellite cells are the catalyst between protein and muscle development.
When you exercise, especially through resistance training, small tears develop in your muscle fibers. Your body responds to these tears by branching together amino acids (the building blocks of protein) together with satellite cells, to repair the tears and make the muscle stronger.
This process requires both adequate dietary protein and resistance training.
What does that have to do with insulin resistance treatment?
Earlier we talked about how glucose is converted to ATP in the mitochondria of the cells. You might remember from middle school science class that the mitochondria are known as the “power house” of the cell.
Here’s where it connects to insulin resistance treatment >>> Resistance training stimulates mitochondrial biogenesis - meaning the creation of more mitochondria - within muscle cells. This is due to the increased need for energy when building and using muscles.
Thus… increased mitochondria = increased need for glucose to create energy = increased glucose uptake into muscle cells.
In fact, it’s important to remember that the research has been clear for years, that as we age, muscle tissue degrades, a condition called sarcopenia. Resistance training has been shown to prevent sarcopenia and improve insulin resistance [1].
all proteins are not created equal
There’s a lot of push from wellness influencers for more women to eat more protein - and they are not wrong (as you can see from our previous discussion).
Protein is needed for nutrient transfer into cells, for neurotransmitter synthesis (mood and sleep regulation), muscle building, and many more reactive and enzymatic processes throughout the body.
What those influencers are not telling you is that the quality of protein matters. Big time.
Having a shelf stocked with protein powders, bars, shakes, and cereals all touting that they are “protein-packed”, you might be missing the mark - especially if those products are made with plant-based proteins.
A FEW THINGS YOU MAY NOT KNOW ABOUT PROTEIN:
plant-based proteins cannot be absorbed and utilized in the body as efficiently as animal proteins [2]
eating more protein can increase health concerns if you have digestive symptoms
in addition to reduced bioavailability, you cannot meet optimal protein intake goals from plant-based sources without also consuming loads of starchy carbohydrates and extra calories - this works against your efforts to resolve insulin resistance symptoms
there are nine amino acids that the human body requires, but cannot make for itself - these are called essential amino acids
it’s important to consume a wide variety of proteins (as well as other foods) to ensure you are getting all essential nutrients required by the body. Additionally, eating the same foods every day is a great way to develop food sensitivities.
EXAMPLE: You would have to consume 700 grams of boiled chickpeas, which contain all nine essential amino acids, to meet your protein intake goals for one day. That’s also 1200 calories, and over 140 grams of starchy carbohydrates. Quinoa and soybeans have similar profiles - imagine eating 6 cups of quinoa to meet your protein intake goals!
MY TAKE ON THE ENVIRONMENTAL IMPACTS OF ANIMAL PROTEINS
TL;DR
Opting out of meat and consuming only plants is not the answer to addressing environmental distress, and especially not your physical health. If your resources allow, consider supporting the farmers who are doing the work to improve environmental impact, so that down the road, this will be more accessible to everyone.
THE DIRT
I greatly value the health of our environment, and do everything within my power to make it better for the next generation. Because of that, I have done a lot of research on the impacts of farming, both livestock and plants, on the environment, and a few things have become very clear:
regenerative farming techniques are showing robust evidence that they actually improve soil quality and sequester carbon - we need to change the way we farm animals, not do away with them altogether. You can help by actively supporting the farmers who are doing this work.
the information being presented in documentaries like [unnamed] has been wildly misrepresented - I urge you to look at the research for yourself.
the amount of waste that comes from processed foods like cereals and plant-based meats is astounding and has a significant impact on environmental health just as much as conventional animal farming. Subsidized grain farms have tilled the soil to the point of desertification, and it needs to stop. Cutting out meat is not the answer.
more ways to improve insulin resistance symptoms
Building muscle is not the only way to combat the effects of insulin resistance. Improving insulin sensitivity is not difficult, but it requires consistency. Here are a few ideas to get you started:
STOP SNACKING
The good news is, increasing protein intake with each meal will help keep you fuller for longer periods of time. When my clients add more protein to their diets, they effectively stop snacking, too. This will help steady your blood glucose levels throughout the day, rather than continuously creating glucose spikes that perpetuate insulin resistance symptoms.
ALTERNATE DAY FASTING
The effects of alternate-day fasting on improving insulin sensitivity are astounding. Not only does fasting increase growth factors that help you build muscle, but when done properly, it increases the sensitivity of your insulin receptors, and helps your body to adapt to using fat for fuel when glucose is not available. It’s extremely important to note that refeeding after fasting is an important part of the process, and learning to fast for health effects is essential. Click here to learn how to fast safely and healthfully.
IMPROVE YOUR MACRONUTRIENT BALANCE
If you’re getting all your protein from a shake stuffed with pea protein isolates, you are doing your body a disservice. Use this guide to build healthier meals that give your body everything it needs to keep you fueled.
FIND AND ADDRESS UNDERLYING CAUSES OF STRESS
Chronic stress, whether from work, relationships, lack of boundaries, or underlying dysfunction in the body, drives insulin resistance and inflammation. Finding and addressing underlying causes of stress, such as digestive dysfunction, adrenal fatigue, or pathogenic infection from yeast overgrowth, parasites, or bacteria, can be pivotal to your insulin resistance treatment. Here’s how I can help.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
The Heart of Physiological Reports - Lindsey - 2024 - Physiological Reports - Wiley Online Library, physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.15962. Accessed 3 Oct. 2025.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.