Boost Your Metabolic Rate with Functional Health
When you feel out of control of your weight, hormones, and eating habits, those one-stop-shop ads and fitness influencers are really appealing. You stopped on this article because (shocker!) those quick fixes and trendy gadgets - the supplement packs, the “metabolic reset diets”, the apple cider vinegar dose, continuous glucose monitors - just aren’t cutting it, and you’re feeling lost and frustrated.
I’ve got you. Improving your metabolic issues is not a quick fix (don’t panic!), but it is possible.
5 Simple Tools to Boost Metabolism - for Good
When you feel out of control of your weight, hormones, and eating habits, those one-stop-shop ads and fitness influencers are really appealing. You stopped on this article because (shocker!) those quick fixes and trendy gadgets - the supplement packs, the “metabolic reset diets”, the apple cider vinegar dose, continuous glucose monitors - just aren’t cutting it, and you’re feeling lost and frustrated.
I’ve got you. Improving your metabolic issues is not a quick fix (don’t panic!), but it is possible - and it’s also FREE - no need to spend loads of cash on trendy gadgets. In this article, I’m going to share my best root-cause fixes to help you regain control of your weight and ditch the diabetic diets for good.
Hi kittens. I’m Hilary Beckwith, ex-dieter and functional nutrition expert. Women with PCOS or who are in perimenopause come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and how their body actually feels. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is metabolism?
reasons you might be gaining weight (or struggle to lose it)
why the quick fixes and trendy gadgets are not the solution to your metabolic issues
5 science-backed tips to improve metabolism from the ground up
what is metabolism?
I hear the term metabolism commonly - and incorrectly - referred to as one’s ability (or inability) to lose weight or burn calories. It kinda makes sense, after all, to turn food into nutrients and eliminate waste is a sort of form of metabolism. In fact, some would refer to this as metabolic rate.
The fact is, your metabolism and weight gain have very little to do with how many or how few calories you consume. In fact, calorie restriction has been shown to slow metabolism over time [1].
“I eat like a bird, and I still gain weight!” I often hear.
The term metabolism refers to your body’s ability or inability to metabolize glucose into energy. One big side effect of a struggling metabolism is, in fact, weight gain - but metabolism has nothing to do with how easily you burn calories.
And as you approach these perimenopause years, the methods that used to work for you no longer do. I can help.
METABOLISM EXPLAINED
In short, glucose is the molecular form of sugar that is used to create energy within the mitochondria of cells in the form of ATP, or Adenosine TriPhosphate. Glucose is broken down from all types of carbohydrates, including starchy vegetables, legumes, grains, and yes, sugars. To some extent, glucose can also come from proteins and fat in someone who has a healthy metabolic flexibility.
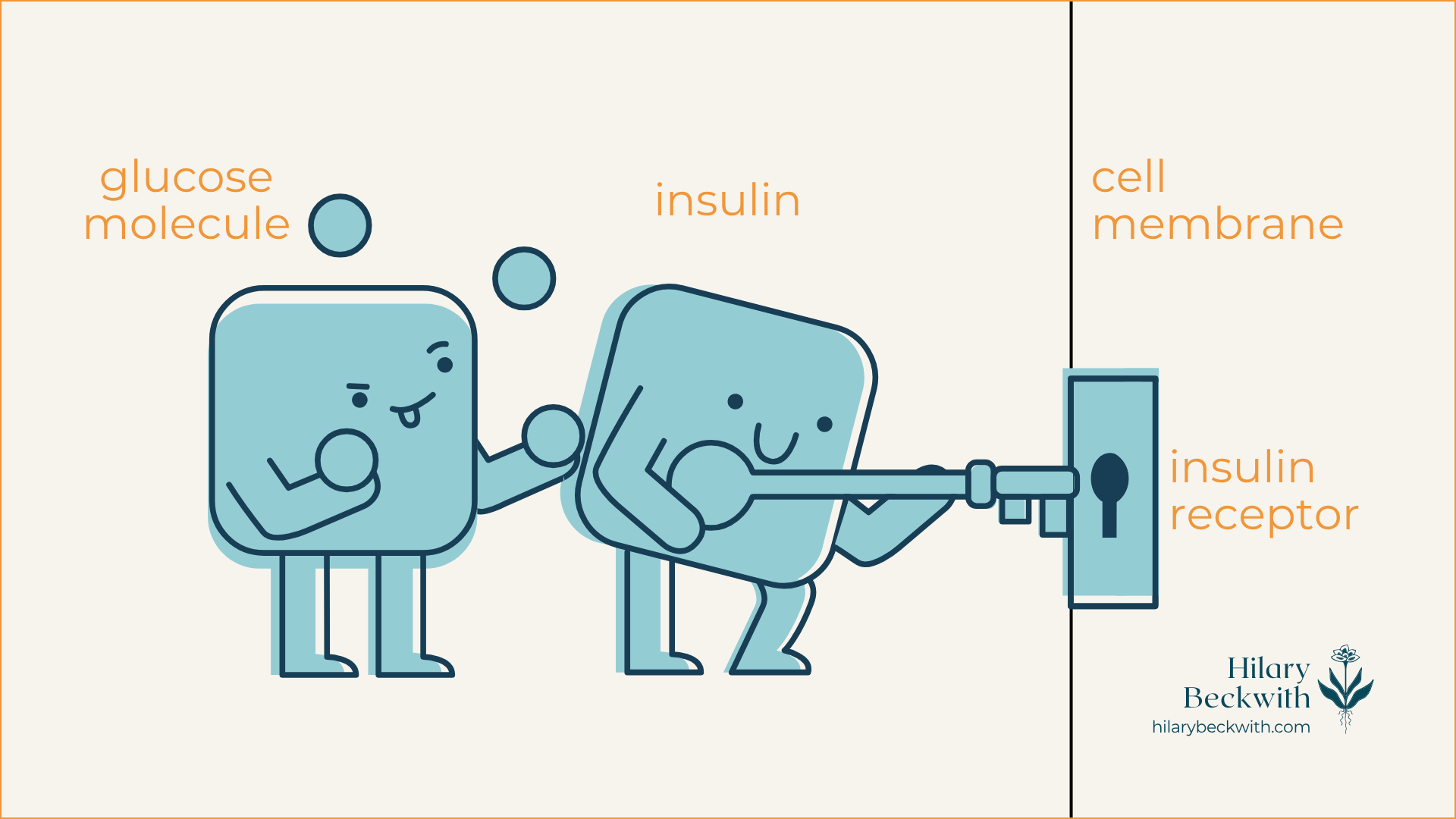
When dietary carbohydrates are broken down into glucose, insulin from the pancreas acts as a key-holder that unlocks the door to the cell (insulin receptor) and shuttles glucose in for energy production. Once cells have had their fill, the remaining glucose is converted into stored forms of glucose and stored in the liver and fat tissue.
non-calorie causes of slow metabolism and weight gain
You read earlier that excess glucose that cannot be used to create ATP is stored as fat tissue, so diet is certainly a factor in metabolism - but it’s not about how many calories are consumed.
In fact, did you know that carbohydrates have less than half the calories per gram than fat does? And yet, it’s not dietary fat that’s causing you to gain weight - it’s carbohydrates.
Wait, wait, WAIT, Hilary - I thought you were anti-diet…
I WANT TO BE VERY CLEAR - I am not villainizing carbohydrates. I love carbs, and our bodies need a balance of macronutrients, including carbohydrates. But for the sake of understanding metabolism and why you are struggling with weight loss, it’s important to understand the health effects of a high-starch or high-carbohydrate diet, in conjunction with a lack of quality protein and fat. And it is especially important to understand that health and weight loss should always be addressed based on the unique needs of each individual.
4 COMMON CAUSES OF WEIGHT GAIN THAT OFTEN GET OVERLOOKED
INSULIN RESISTANCE - This is metabolism at its core - if your cells shut out insulin, your metabolism will struggle, and you will gain weight as fat (more on this later). This is often caused by diet, low muscle tone, as well as the depletion of estrogen during perimenopause, which causes a major decline in insulin sensitivity.
UNADDRESSED GUT PATHOGENS - Overgrown pathogens in the gut, like yeast, bacteria, h. pylori (also a bacteria, but found in the stomach), mold, or parasites (yes, parasites!), will cause the body to inhibit the breakdown of fat (lipolysis).
PROLONGED INFECTIONS - Infections like the ones just discussed will cause the liver to release more fat and sugars into the bloodstream, encouraging the body to store more fat. Additionally, these infections cause the body to preserve calories for immune function, rather than energy production.
PROCESSED FOODS (I know…) - When your body doesn’t know what to do with something, it stores it as fat. Binders, fillers, chemicals, preservatives, and plastics from processed food products must all be dealt with by the liver, neutralized, and eliminated. When the liver is overburdened and elimination pathways are not clear, these products remain in the body and get stored in fat tissue. Your body will make more fat tissue to accommodate these storage needs.
This is exactly why the expensive, trendy gadgets are not the solution to your metabolic health. Let’s dig into it more.
improving metabolic health is free
You do not need the expensive, trendy gadgets and trackers to improve metabolic health. I know the ads and influencers can be very convincing, and there can be some value in the data they provide.
However…
Most often, what I see with clients who use gadgets like CGMs (continuous glucose monitors), Aura rings, sleep apps, calorie-tracking apps, and other wearables is an obsession over fixing the data, rather than a tool for understanding. This is a form of disordered eating behavior known as orthorexia.
They disconnect from what their body actually needs, and obsess over food restrictions and looking at the data. In doing so, they become less present with themselves and others, and they begin to loathe food, rather than enjoy it.
Sure, that CGM is helpful to understanding which foods have a negative impact on blood sugar, but finding and addressing the root causes of the blood sugar dysregulation is far more effective long-term than obsessively chasing numbers.
5 ways to improve metabolic health - for good
I want to be clear - I do not believe weight is an indicator of health. I never ask my clients to step on a scale, and I am a Health At Every Size (HAES) advocate. I firmly believe that all bodies can be healthy.
But, as someone who grew up in what I call the Fat-Free Era, obsessed about my body shape and size, shrunken with shame, and and shrouded in disordered eating behaviors, I know what it can feel like to have this weight creep on without explanation, and feel out of control - or worse - like I did something wrong (thanks, trauma!).
I’m not here to tell you you need to lose weight - I am here to help you make sense of your metabolic health so you can feel more in control of your health, and reconnect with your body’s needs.
With that, here are 5 ways to improve metabolic health from the ground up:
PRIORITIZE STRENGTH + RESISTANCE TRAINING OVER CARDIO
Building muscle is essential to improving insulin sensitivity, and involves regular lifting and adequate consumption of quality protein - especially in perimenopause and post-menopause years. Yes, endurance cardio can be more effective at burning fat, but that does not improve insulin resistance in the long term, whereas strength training does. CLICK HERE to read more about how protein and muscle building improve insulin sensitivity and metabolic issues.
PRIORITIZE SLEEP
Yes, really! Sleep is when your body does most of its healing and detoxifying, which, as you learned earlier, plays a significant role in how your body makes, metabolizes, and stores fat. Sleep is when your brain sweeps out toxic byproducts from the day’s events, it’s when your liver function is at its highest, and when tissues heal. CLICK HERE to learn more about managing sleep and stress.
INCORPORATE A (SAFE) FASTING ROUTINE
Fasting is not something everyone should do. And it certainly isn’t something anyone should jump into, feet first. But fasting has immense benefits on cellular health, gut health (including the clearing of pathogens we discussed earlier), improves insulin sensitivity, and improves metabolic flexibility, which helps your body adapt to burning fat when glucose stores are low. And the most important part about fasting when it comes to addressing metabolic issues - is what you eat AFTER you fast. CLICK HERE to learn more about how to fast, when to fast, who should (and should not) fast, and how to refeed your body after a fast to support healthy metabolism.
PRIORITIZE WHOLE FOODS (AND LEARN TO SPOT HEALTH SCAMS ON PACKAGED FOODS)
Working in functional nutrition, I often see that clients are confused about what is healthy and what is not, because MARKETING. Food marketers are paid to get you to buy their product - period. That said, there are so many foods marketed as being “healthy” that are still just processed garbage. Not all packaged foods are bad, but the easiest way to remove processed foods and improve your metabolic issues is to prioritize whole foods over packaged. And because that isn’t always the easiest option for someone who is very busy or isn’t comfortable in the kitchen, I've developed this online course to help you learn what to look for on ingredient lists so you can make the best choice for your body.
PRIORITIZE QUALITY PROTEIN AND NON-STARCHY VEGETABLES AT EVERY MEAL
Making protein and fiber a priority at every meal is one of the easiest ways to improve metabolic issues. Smoked salmon on a bed of greens and sauerkraut for breakfast, grass-fed beef stir-fry over cauliflower rice and lots of veg for lunch, and maple-mustard roast chicken and veg for dinner. Prioritizing protein and non-starchy veg keeps you full for longer periods of time and improves your metabolic flexibility and sugar cravings. CLICK HERE to read more about the importance of protein.
was this helpful?
Please share your thoughts and questions in the comments below.
Want options for finding and addressing the gut pathogens discussed earlier?
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Knuth ND;Johannsen DL;Tamboli RA;Marks-Shulman PA;Huizenga R;Chen KY;Abumrad NN;Ravussin E;Hall KD; “Metabolic Adaptation Following Massive Weight Loss Is Related to the Degree of Energy Imbalance and Changes in Circulating Leptin.” Obesity (Silver Spring, Md.), U.S. National Library of Medicine, pubmed.ncbi.nlm.nih.gov/25236175/. Accessed 19 Nov. 2025.
3 Reasons I Do Not Recommend a Vegetarian or Vegan Diet - Seattle Nutrition Blog
f insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
My Clients Get Better Results with Animal Proteins
When women come to me with symptoms like sleep issues, sugar cravings, and irregular periods or a PCOS diagnosis, my first thought is adrenal fatigue. Adrenal symptoms like these are often paired with prolonged chronic stress, blood sugar dysregulation, and insulin resistance.
Which leads me to the question - are these women getting enough quality protein? In an effort to marry two articles I’ve previously written on the role of protein in insulin resistance, and the health effects of a vegan diet, I’m bringing these two ideas together to help you see the full picture.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
why protein matters
why I won’t work with clients who are unwilling to include animal proteins in their diet
what is insulin resistance?
In short, glucose is the molecular form of sugar that is used to create energy within the mitochondria of cells in the form of ATP, or Adenosine TriPhosphate. Glucose is broken down from all types of carbohydrates, including starchy vegetables, legumes, grains, and yes, sugars.
When dietary carbohydrates are broken down into glucose, insulin from the pancreas acts as a key-holder that unlocks the door to the cell (insulin receptor) and shuttles glucose in for energy production. Once cells have had their fill, the remaining glucose is converted into stored forms of glucose and stored in the liver and fat tissue.
For someone who regularly consumes carbohydrate-rich meals and snacks, there is often more glucose in their bloodstream than cells can handle. This causes cells to deactivate their insulin receptors, sending the message, “we’ve had enough!”.
This deactivation of insulin receptors is known as insulin resistance, and it becomes a problem that perpetuates itself until meaningful dietary and lifestyle changes are made.
why protein matters
Dietary protein is essential to many biological functions. It’s needed for nutrient transport across cell membranes, used in the formation of antibodies, needed for neurotransmitter formation which impacts mood and sleep, and it’s needed to strengthen muscles.
Most of us don’t get enough protein daily. In fact the current Recommended Dietary Allowance (RDA) for protein was decided in 1989, and is considered the minimum needed to maintain health in sedentary individuals [1], not what is best for optimal health and activity levels. The RDA for protein is 0.75g per 1kg of body weight.
For a female-bodied individual weighing 150lbs (68kg), the RDA is 51g protein daily. More current research has found that higher protein intake is more conducive to optimal health and should be considered over the current RDA [2}.
If you are the person whose shelves are loaded with “protein-packed” packaged snacks, vegan protein powders, or if you came here searching for vegetarian high-protein recipes, consider this: Plant proteins and animal proteins are not equally absorbed and used by human bodies [3].
Don’t take my word for it - read the research for yourself.
HERE’S WHERE IT CAN GO WRONG
If insulin resistance is primarily caused and perpetuated by a carbohydrate-rich diet, consider this: You cannot reach optimal dietary protein goals from a vegan or vegetarian diet without also consuming mountains of starchy carbohydrates and loads of extra calories.
My clients often require a daily protein intake of about 100g (depending on the individual’s body size, activity, and digestive health). This breaks down to roughly 30-35g of protein per meal.
You would have to consume 4 cups of cooked quinoa to meet that requirement for one meal.
Here are some additional protein source comparisons:
2 cans chickpeas (drained) = 704 calories + 36g protein
3/4 block tofu = 266 calories + 31.8g protein
4 cups cooked quinoa = 888 calories + 32.8g protein
4oz grass-fed beef = 157 calories + 24g protein (plus grass-fed beef is shown to have a more dense nutrient profile than conventional beef, including significantly higher levels of superoxide dismutase and Omega 3 fatty acids)
1/2 fillet wild-caught salmon = 209 calories + 31g protein
5 large eggs = 360 calories + 31.5g protein
1 chicken breast (120g) = 198 calories + 37g protein
This lack of protein, paired with carbohydrate-rich eating habits is also a major driver of pathogenic infections, such as candida or yeast overgrowth, small intestinal bacterial overgrowth (SIBO), and can impair digestive function over time, increasing susceptibility for parasite and helicobacter pylori infections as well. I’ll explain more of this mechanism later in the post.
why i don’t work with clients who are unwilling to consume animal proteins
The short answer - their success and my reputation depend on it.
I have worked with clients in the past who prefer vegetarian and vegan diets, and the reality is - they do not celebrate the same successes that my omnivorous clients do when it comes to resolving their digestive symptoms, PCOS symptoms, and weight issues.
If that sounds too harsh, please know that I do hold space for different views on vegetarian vs vegan vs omnivorous diets, and can appreciate that there are many different reasons for choosing one over another.
This decision does not come from a place of judgment, but rather for the sake of the long-term health and success of the women who come to see me.
When it comes to symptoms of hormone imbalance, sleep issues, blood sugar management issues, weight loss, and irregular periods, a diet without animal proteins simply will not support their efforts to address symptoms.
Here’s where I see the biggest impacts.
HORMONE HEALTH
The women and female-bodied individuals who come to see me, often present with symptoms of hormone imbalance, be it a PCOS diagnosis, irregular periods, PMS symptoms, painful periods, mood and sleep disruptions around their periods, migraines around their periods, and weight gain in their belly or hips.
Aside from the obvious ovaries, hormones are largely modulated by the adrenal glands and the liver. The adrenal glands are responsible for producing any sex hormones that are not produced by the ovaries or testes, and the liver is charged with hormone balance, in that, it is responsible for deactivating and eliminating excess hormones to maintain balance.
A diet rich in carbohydrates, and especially low in protein, drives insulin resistance which disrupts the HPA (hypothalamus, pituitary, adrenal) axis and consequently, the ability of the ovaries and adrenal glands to produce hormones.
Additionally, when left unaddressed, this disruption leads to prolonged chronic stress, leading to adrenal fatigue, chronic inflammation, and abnormal thyroid labs. This is a highly complex topic that I go into more detail about here.
Finally, a liver that is overburdened with the job of constantly having to convert excess glucose into fat and glycogen may not be able to effectively metabolize and eliminate excess hormones well, exacerbating hormone imbalance symptoms.
BLOOD SUGAR BALANCE
If you wake up around 2:00 am most nights to pee, or get “hangry” between meals, you have blood sugar regulation issues. This, too, involves your liver and adrenal glands, and is highly driven by a carbohydrate-rich diet, among other things.
Additionally, carb and sugar cravings are common symptoms of the pathogenic infections we discussed earlier. You see, yeast and bacteria LOVE sugar, and when they infiltrate your gut, they live off of your resources. This perpetuates blood sugar imbalances, leading to insulin resistance, adrenal fatigue, and symptoms of hormone imbalance. (seeing a pattern here?)
GUT HEALTH
This topic is multifaceted, but here are the two main points I want to focus on for the sake of this post:
lack of protein inhibits digestion - Healthy digestion relies on many components - a regulated nervous system, optimal output of digestive juices (enzymes and stomach acid), and adequate chewing and mechanical digestion. Consuming protein tells your body to produce stomach acid (HCl) and proteolytic enzymes. With a low-protein diet, HCl production suffers, and so does your digestion. Since one of the main roles of HCl is to disinfect your food, poor HCl output leaves you more susceptible to pathogenic infections of the gut, driving inflammation, hormone issues, and overall discomfort.
migrating motor complex (MMC) - This important mechanism occurs only in a fasted state, and consists of a cascade of events intended to sweep out unwanted microbes from the small intestine. A carbohydrate-rich diet often makes one hungry more frequently throughout the day, leaving very little fasted time for the MMC to activate. If you are one who snacks or grazes throughout the day, you are doing your gut a disservice.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
National Research Council (US) Subcommittee on the Tenth Edition of the Recommended Dietary Allowances. “Protein and Amino Acids.” Recommended Dietary Allowances: 10th Edition., U.S. National Library of Medicine, 1 Jan. 1989, www.ncbi.nlm.nih.gov/books/NBK234922/.
Hudson, Joshua L, et al. “Protein Intake Greater than the RDA Differentially Influences Whole-Body Lean Mass Responses to Purposeful Catabolic and Anabolic Stressors: A Systematic Review and Meta-Analysis.” Advances in Nutrition (Bethesda, Md.), U.S. National Library of Medicine, 1 May 2020, pmc.ncbi.nlm.nih.gov/articles/PMC7231581/.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.
The Role of Protein in Insulin Resistance Symptoms and Treatment
And still, you've bought into vegan protein shakes, and have shelves loaded with protein-enriched cookies, bars, and cereals. You’re feeling pretty good about meeting those higher protein intake recommendations that saturate your social feed.
But I’m here to dig deeper into the role of protein in insulin resistance symptoms, and why getting your protein from those sources might be making your insulin resistance symptoms worse, contributing to weight gain and inflammation.
The role of protein in insulin resistance treatment
If you’ve followed me for any amount of time, you know that what’s missing from those posts from fitness influencers you follow on TikTok, is nuance. That’s what I bring to the table.
You might have already read my articles about protein quality and the health effects of a vegan diet. And still, you've bought into vegan protein shakes, and have shelves loaded with protein-enriched cookies, bars, and cereals. You’re feeling pretty good about meeting those higher protein intake recommendations that saturate your social feed.
But I’m here to dig deeper into the role of protein in insulin resistance symptoms, and why getting your protein from those sources might be making your insulin resistance symptoms worse, contributing to weight gain and inflammation.
Hi darlings. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress, insulin resistance, and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between their lab values and what their body is saying. Before you continue, click here to read my Medical Disclaimer.
In this article, you’ll learn:
what is insulin resistance?
insulin resistance causes and symptoms
the role of protein in insulin resistance treatment
why protein quality matters just as much as quantity
more ways to improve insulin sensitivity symptoms
what is insulin resistance?
The word metabolism often gets referred to as one’s ability or inability to lose weight. But the word metabolism actually refers to the conversion of one component into another.
With digestion, metabolism might refer to ingested food being broken down into nutrients your body can use. Or a chemical component of medication or a food additive might be manipulated by enzymes into a neutralized form and removed from the body.
For the sake of this discussion, we’ll be referring to metabolism in regard to glucose metabolism - the conversion of glucose (a molecular form of sugar) into energy or fat.
It’s important to understand that glucose comes from more than just sugar ingredients. Glucose comes from all carbohydrates, including grains, starches, and yes, sugar.
So, whether it’s potatoes, sweet potatoes, rice, bread, legumes, fruit, honey, or candy - it all turns into glucose.
And that glucose either gets metabolized into energy or fat. Insulin, a hormone produced by the pancreas, is required for the metabolism of glucose into energy.
Here’s how glucose metabolism works:
When you consume any kind of carbohydrate, be it starchy legumes, grains, or vegetables, sugars like honey, fruit, or cane sugar, even leafy greens contain carbohydrates - those carbohydrates are broken down into molecules called glucose.
Glucose molecules are transported into your bloodstream through the epithelial lining of the small intestine. The amount of glucose molecules in your bloodstream at any given time is referred to as your “blood sugar” or “blood glucose” level.
Insulin is released by the pancreas and acts as sort of an usher, taking the glucose to individual cells, and using its key to unlock the door (insulin receptors embedded in the cell membrane) and shuttles the glucose in to be metabolized (hey, there’s that word again!) via the Krebs cycle within the mitochondria.
When cells have had their fill of glucose, any glucose remaining is then sent to the liver and converted to storable forms of glucose, specifically glycogen and triglycerides.
Glycogen: stored primarily in the liver, and to some extent, muscles. The liver has a very small capacity for glycogen storage.
Triglycerides: stored as fat tissue, also called adipose tissue. Your body has unlimited stores of triglycerides in adipose tissue, as it can always (and does) make more fat to accommodate more triglyceride storage.
HERE’S WHERE THINGS CAN GO WRONG
Insulin resistance occurs when there is regularly more glucose than can be used by cells in the bloodstream. For example, one who consumes a high-carbohydrate diet at most meals and snacks will likely develop insulin resistance symptoms.
When there is regularly more glucose in the bloodstream than cells can accommodate, insulin receptors (remember the locked doors on cell membranes) begin to deactivate, making insulin ineffective. The cells are essentially saying, “we’ve had enough!”.
In response, the body produces more insulin to try and compensate for glucose not getting into cells, and as a result, insulin resistance worsens.
And what happens to glucose that does not enter cells? It gets converted to fat.
insulin resistance causes and symptoms
COMMON CAUSES OF INSULIN RESISTANCE
high starch, high carbohydrate diet
regular consumption of processed foods (including foods you might consider “health foods”, like protein powders, bars, shakes, and plant-based meat substitutes)
chronic stress (external or internal) - Click here to read more about the role of cortisol in blood sugar regulation
inactivity/sedentarianism
inadequate sleep
overexercising (especially cardio)
pancreatic insufficiency (more on what symptoms look like later in the article)
leaky gut syndrome
COMMON SYMPTOMS OF INSULIN RESISTANCE
weight gain in belly and/or hips
difficulty losing weight
“hangry” symptoms between meals (loss of focus, shaky, irritability)
digestive symptoms
pancreatic insufficiency can often contribute to digestive dysfunction, as it is needed to produce digestive enzymes
digestive symptoms are often indicative of pathogenic infection, such as yeast or bacterial overgrowth, mold, or parasites - all of which contribute to chronic stress response and cortisol output
excess hunger (frequent hunger, or excess appetite)
Type II Diabetes diagnosis, or pre-diabetes
abnormal thyroid labs (click here to read more)
sweet, salty, or carb cravings
the role of protein in insulin resistance treatment
It’s no secret that we need protein to build muscle - and that’s exactly the same reason it’s needed for insulin resistance treatment.
Let me explain.
HOW YOUR BODY BUILDS MUSCLES
A common misconception about building muscles, is that it requires an increase in the number of muscle cells (also called muscle fibers) - but this is incorrect. Your body actually cannot produce more muscle cells.
Muscle cells can, however, get larger in size - this is what is known as hypertrophy.
Additionally, contained in the fluid between muscle cells are smaller stem cells called satellite cells. In addition to hypertrophy, the satellite cells are the catalyst between protein and muscle development.
When you exercise, especially through resistance training, small tears develop in your muscle fibers. Your body responds to these tears by branching together amino acids (the building blocks of protein) together with satellite cells, to repair the tears and make the muscle stronger.
This process requires both adequate dietary protein and resistance training.
What does that have to do with insulin resistance treatment?
Earlier we talked about how glucose is converted to ATP in the mitochondria of the cells. You might remember from middle school science class that the mitochondria are known as the “power house” of the cell.
Here’s where it connects to insulin resistance treatment >>> Resistance training stimulates mitochondrial biogenesis - meaning the creation of more mitochondria - within muscle cells. This is due to the increased need for energy when building and using muscles.
Thus… increased mitochondria = increased need for glucose to create energy = increased glucose uptake into muscle cells.
In fact, it’s important to remember that the research has been clear for years, that as we age, muscle tissue degrades, a condition called sarcopenia. Resistance training has been shown to prevent sarcopenia and improve insulin resistance [1].
all proteins are not created equal
There’s a lot of push from wellness influencers for more women to eat more protein - and they are not wrong (as you can see from our previous discussion).
Protein is needed for nutrient transfer into cells, for neurotransmitter synthesis (mood and sleep regulation), muscle building, and many more reactive and enzymatic processes throughout the body.
What those influencers are not telling you is that the quality of protein matters. Big time.
Having a shelf stocked with protein powders, bars, shakes, and cereals all touting that they are “protein-packed”, you might be missing the mark - especially if those products are made with plant-based proteins.
A FEW THINGS YOU MAY NOT KNOW ABOUT PROTEIN:
plant-based proteins cannot be absorbed and utilized in the body as efficiently as animal proteins [2]
eating more protein can increase health concerns if you have digestive symptoms
in addition to reduced bioavailability, you cannot meet optimal protein intake goals from plant-based sources without also consuming loads of starchy carbohydrates and extra calories - this works against your efforts to resolve insulin resistance symptoms
there are nine amino acids that the human body requires, but cannot make for itself - these are called essential amino acids
it’s important to consume a wide variety of proteins (as well as other foods) to ensure you are getting all essential nutrients required by the body. Additionally, eating the same foods every day is a great way to develop food sensitivities.
EXAMPLE: You would have to consume 700 grams of boiled chickpeas, which contain all nine essential amino acids, to meet your protein intake goals for one day. That’s also 1200 calories, and over 140 grams of starchy carbohydrates. Quinoa and soybeans have similar profiles - imagine eating 6 cups of quinoa to meet your protein intake goals!
MY TAKE ON THE ENVIRONMENTAL IMPACTS OF ANIMAL PROTEINS
TL;DR
Opting out of meat and consuming only plants is not the answer to addressing environmental distress, and especially not your physical health. If your resources allow, consider supporting the farmers who are doing the work to improve environmental impact, so that down the road, this will be more accessible to everyone.
THE DIRT
I greatly value the health of our environment, and do everything within my power to make it better for the next generation. Because of that, I have done a lot of research on the impacts of farming, both livestock and plants, on the environment, and a few things have become very clear:
regenerative farming techniques are showing robust evidence that they actually improve soil quality and sequester carbon - we need to change the way we farm animals, not do away with them altogether. You can help by actively supporting the farmers who are doing this work.
the information being presented in documentaries like [unnamed] has been wildly misrepresented - I urge you to look at the research for yourself.
the amount of waste that comes from processed foods like cereals and plant-based meats is astounding and has a significant impact on environmental health just as much as conventional animal farming. Subsidized grain farms have tilled the soil to the point of desertification, and it needs to stop. Cutting out meat is not the answer.
more ways to improve insulin resistance symptoms
Building muscle is not the only way to combat the effects of insulin resistance. Improving insulin sensitivity is not difficult, but it requires consistency. Here are a few ideas to get you started:
STOP SNACKING
The good news is, increasing protein intake with each meal will help keep you fuller for longer periods of time. When my clients add more protein to their diets, they effectively stop snacking, too. This will help steady your blood glucose levels throughout the day, rather than continuously creating glucose spikes that perpetuate insulin resistance symptoms.
ALTERNATE DAY FASTING
The effects of alternate-day fasting on improving insulin sensitivity are astounding. Not only does fasting increase growth factors that help you build muscle, but when done properly, it increases the sensitivity of your insulin receptors, and helps your body to adapt to using fat for fuel when glucose is not available. It’s extremely important to note that refeeding after fasting is an important part of the process, and learning to fast for health effects is essential. Click here to learn how to fast safely and healthfully.
IMPROVE YOUR MACRONUTRIENT BALANCE
If you’re getting all your protein from a shake stuffed with pea protein isolates, you are doing your body a disservice. Use this guide to build healthier meals that give your body everything it needs to keep you fueled.
FIND AND ADDRESS UNDERLYING CAUSES OF STRESS
Chronic stress, whether from work, relationships, lack of boundaries, or underlying dysfunction in the body, drives insulin resistance and inflammation. Finding and addressing underlying causes of stress, such as digestive dysfunction, adrenal fatigue, or pathogenic infection from yeast overgrowth, parasites, or bacteria, can be pivotal to your insulin resistance treatment. Here’s how I can help.
learn something new?
Please share your thoughts and questions in the comments below.
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
The Heart of Physiological Reports - Lindsey - 2024 - Physiological Reports - Wiley Online Library, physoc.onlinelibrary.wiley.com/doi/10.14814/phy2.15962. Accessed 3 Oct. 2025.
Association of Major Dietary Protein Sources with All‐cause and Cause‐specific Mortality: Prospective Cohort Study | Journal of the American Heart Association, www.ahajournals.org/doi/10.1161/JAHA.119.015553. Accessed 3 Oct. 2025.
Intermittent Fasting for Metabolic Rate and Weight Loss
If you get the majority of your health information from fitness and wellness influencers on Instagram or TikTok, you might be getting misinformation about intermittent fasting benefits.
When done properly, fasting and intermittent fasting will improve insulin resistance, metabolic rate, and metabolic flexibility, regardless of the number of calories consumed before and after fasting. If you think of fasting as an easy way to achieve a calorie deficit, think again.
Fasting benefits for insulin resistance and metabolic rate - not calorie restriction
If you get the majority of your health information from fitness and wellness influencers on Instagram or TikTok, you might be getting misinformation about intermittent fasting benefits.
When done properly, fasting and intermittent fasting will improve insulin resistance, metabolic rate, and metabolic flexibility, regardless of the number of calories consumed before and after fasting. If you think of fasting as an easy way to achieve a calorie deficit, think again.
Hi friends. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively and fill in the gaps between what their doctor is saying and what their body is saying. Click here to read my Medical Disclaimer.
In this article, you’ll learn:
the difference between calorie deficit and intermittent fasting
physiological effects of fasting
different types of fasting
what should you eat to break your fast?
who should not practice fasting?
isn’t fasting just another way to restrict calories?
Yes and no.
The research behind fasting and metabolic rate tells us two main key points:
chronic calorie restriction (dieting) slows metabolism over time [1,2], and
the chronic presence of insulin slows metabolism, causes weight gain, and increases insulin resistance [3,4]
And since insulin is released in times of feeding, especially carbohydrates (fibers, starches, and sugars), it can be said that calorie restriction is a part of the world of fasting benefits - but not for the sake of achieving a calorie deficit.
EXAMPLES OF CALORIE RESTRICTION V. FASTING FOR INSULIN RESISTANCE
SCENARIO #1: Using the Calorie Restriction (Dieting) Method for Weight Loss
You decide to use the calorie deficit method for weight loss, meaning, the calories you burn must be more than the calories you consume. This requires avid tracking on your part, a constant attention to calorie count and scale numbers, and even then you are missing important data - your total energy expenditure, which varies widely from person to person, and requires a very specialized type of testing.
You increase calorie burn at the gym, and decrease calorie consumption. You track it meticulously using calorie deficit calculators and apps, and find you lose weight for the first 3-4 weeks of doing it. Then you plateau - even when in a calorie deficit, you find the weight is not shedding as easily as it once was. You become discouraged and irritable, and decide to “give in” when things aren’t working any longer.
SCENARIO #2: Intermittent Fasting for Metabolic Rate and Insulin Resistance
You decide to use intermittent fasting (we’ll talk about terminology and semantics later in the post) as a weight loss tool, applying a method commonly known as “16/8”, wherein you consume all your calories within an 8-hour window of time, with nothing but water for the remaining 16 hours of a 24-hour day. You don’t necessarily consume fewer calories, but find that your weight sheds at a slower, more consistent rate, and doesn’t plateau like it does with calorie restriction. You enjoy foods more because you’re eating the calories your body needs, and not restricting food types. You’re not tracking calories, not obsessively looking at numbers on an app or nutrition label. This feels sustainable.
The two main talking points we’ll return to throughout this article are:
the quality of the calorie matters
the timing of calorie consumption matters
your body’s long-term metabolic response to fasting requires time and consistency - one day of fasting is not enough to magically boost your body’s metabolic rate, even if you begin to see weight loss results
how fasting works
In a nutshell, when fasting is done well, the intention of fasting is to reduce the amount of insulin being released into your bloodstream by eliminating food intake for a period of time.
With time and consistency, this method can help improve insulin sensitivity (more on this) and improve your body’s ability to use fat stores when glucose is not readily available. Put differently, proper fasting increases metabolism and improves your body’s ability to burn fat.
To understand how this works, we need to look at how metabolism works. Take a look at the diagram below.
Here are a few key points to understand before we move on to different types of fasting:
WHAT IS METABOLISM?: Metabolism, specifically glucose metabolism, is a cascade of events that converts glucose into energy (ATP or Adenosine TriPhosphate). The process occurs inside of cells, and heavily involves the mitochondria, known as the “powerhouse of the cell” for this very reason - it very literally supplies the power that your cells and body need to function. Your body prioritizes carbohydrates for metabolism, but can also use proteins or fats when resources are present. Because converting fats and protein into ATP requires more energy, the body prioritizes carbohydrate sources of glucose.
WHAT IS GLUCOSE?: Glucose is the molecular form of sugar. Put differently, glucose is sugar in its most broken-down form. Glucose comes primarily from carbohydrates, including starches, sugars, and fiber.
WHAT IS INSULIN?: Insulin is a hormone produced by the pancreas when glucose is present. Insulin acts as a keyholder to cells - when glucose is present, insulin binds to the glucose molecule, shuttles it to the cell, and unlocks the proverbial door, allowing the glucose to enter and be converted to ATP by the mitochondria.
WHAT IS INSULIN RESISTANCE?: When your cells are consistently exposed to more glucose than they can handle, they begin deactivating insulin receptors - if insulin is a key holder, and insulin receptors are the doors to the cell, picture the insulin receptors being boarded up with signs that say “KEEP OUT!”.
Insulin resistance is typically the long-term result of diets low in whole food fiber, high in refined carbohydrates, and snacking or grazing often.
Insulin resistance is common in women with PCOS, hence the belly weight, sugar cravings, and “hangry” symptoms.
In the case of insulin resistance, glucose cannot enter cells to create fuel. The body produces even more insulin in an effort to get the glucose into cells (which does not work).
With or without insulin resistance, any remaining glucose after cells have had their fill gets converted into glycogen (liver storage of glucose) and triglycerides, which get stored as fat tissue.
Improving insulin sensitivity helps your body metabolize glucose more effectively and improves your ability to use fat as a secondary fuel source when glucose is not present. Proper fasting helps improve insulin sensitivity.
types of fasting
As we’ve discussed, fasting is not merely calorie restriction. What you eat before and after fasting, and the timing and quality of your daily meals, are also important factors when it comes to fasting for insulin resistance.
But let’s talk about different fasting terms first, so you can be on the same page as your health practitioners. You can see my earlier writings on fasting benefits here.
INTERMITTENT FASTING: This term is commonly used incorrectly to refer to Time-Restricted Feeding. Here is the correct use of this term: Intermittent Fasting, also known as Alternate-Day Fasting, refers to a water-only fast for 24-72 hours, with careful attention to refeeding after each fast.
TIME-RESTRICTED FEEDING: Again, often mistaken for Intermittent Fasting, but they are two different fasting methods. Time-Restricted Feeding allows you to eat daily, consuming all your calories within a set window of time. Sometimes referred to using the number of hours chosen to consume calories, such as “16/8”, meaning you’d consume all your calories within an 8-hour window, while taking in nothing but water for 16 hours.
EXTENDED FASTING: Water-only fasting that lasts longer than 72 hours.
what should you eat after fasting?
There’s an abundance of poorly researched papers written regarding the long-term effects of fasting. But there’s some really great ones, too, and from credible sources. Many of these studies are discussed in Jason Fung’s The Obesity Code [5].
Some practitioners and influencers across the internet are touting that fasting benefits don’t last once you stop. Here’s why they have it wrong:
Studies that suggest this conclusion also do not disclose the eating and activity habits of the subjects. A study that observes this outcome, but does not provide clear data on all related factors (I would argue that what and when the subject eats is an important determining factor), is not a credible resource.
That said, a regular diet of starches, sugars, and processed foods is bound to undo any work you do with fasting, but the research on fasting benefits is clear:
Water fasting improves insulin sensitivity, increases growth hormone (which also protects from protein degradation), and increases metabolism. You can’t expect to stay healthy on a diet of processed foods, no matter how frequently you fast.
Below are my generally recommended food guidelines for post-fasting, but it’s important to remember that every individual has unique food and macronutrient needs, based on their biochemical composition and unique health goals.
WHAT TO EAT AFTER FASTING:
choose whole foods
prioritize fat, protein, and fiber
avoid highly marketed “health food” labels, like “gluten-free”, “plant-based”, or “[number] essential vitamins” - these are not health foods, and are often highly processed (click here to learn how to spot health scams and confidently read food labels)
don’t be afraid to consume more calories in your fast-break meal than you would typically, but use these techniques to help you avoid overeating:
eat while seated
take a few long, deep breaths through your nose before taking your first bite
take small bites and chew thoroughly (read why this matters)
mindfully eating improves digestion and helps you to listen to when your body is satisfied
MEAL IDEAS FOR POST-FASTING:
Mediterranean Scramble - 3 scrambled eggs, 4-5 olives, 3 ounces plain whole-milk yogurt, and crumbled feta over a handful of chopped, sauteed greens (dandelion, chard, kale, broccolini, beet greens).
Broiled Salmon and Green Vegetable - 5-ounce salmon filet cooked and seasoned to your liking, paired with roasted broccoli, stir-fried asparagus, or sautéed greens. Top with sauerkraut, yogurt, or avocado.
Avocado “Toast” with Poached Eggs and Shredded Beef - Two thin slices of sweet potato baked until tender. Top with mashed avocado, sprouts, 2 poached eggs, and a generous scoop of leftover shredded beef.
While the health benefits of fasting are meaningful, fasting should not be practiced by everyone, and should always be practiced under the supervision of a qualified healthcare practitioner.
If you want to explore fasting for weight loss or metabolic health, click here to book a free consultation so we can talk about it.
was this helpful?
What’s your experience with fasting? Have you found any benefit from fasting?
Share your thoughts and questions in the comments below!
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Zauner, C., Schneeweiss, B., Kranz, A., Madl, C., Ratheiser, K., Kramer, L., Roth, E., Schneider, B., & Lenz, K. (2000). Resting energy expenditure in short-term starvation is increased as a result of an increase in serum norepinephrine. The American journal of clinical nutrition, 71(6), 1511–1515. https://doi.org/10.1093/ajcn/71.6.1511
Most, J., & Redman, L. M. (2020). Impact of calorie restriction on energy metabolism in humans. Experimental gerontology, 133, 110875. https://doi.org/10.1016/j.exger.2020.110875
Kolb, Hubert, et al. “Insulin Translates Unfavourable Lifestyle into Obesity - BMC Medicine.” BioMed Central, BioMed Central, 13 Dec. 2018, bmcmedicine.biomedcentral.com/articles/10.1186/s12916-018-1225-1.
Kahn, B. B., & Flier, J. S. (2000). Obesity and insulin resistance. The Journal of clinical investigation, 106(4), 473–481. https://doi.org/10.1172/JCI10842
Fung, J. (2016). The Obesity Code: Unlocking the Secrets of Weight Loss. Greystone Books.
Symptoms of Hormone Imbalance and Hormone Balancing Supplements
The adrenal glands do not get nearly enough limelight when it comes to addressing hormone imbalance symptoms. Dysfunction in the adrenal glands will disrupt hormone balance and cause issues with sleep, periods, mood, energy, and blood sugar levels.
Addressing adrenal health and stress management are the keys to getting better, more predictable periods, and improving mood and energy levels.
But there’s more to it than bubble baths or meditation.
Stress management and hormone imbalance
You’re gaining weight, you don’t sleep well, your periods are getting progressively off track, and you are desperately trying to find answers.
You go in for your annual bloodwork and ask your physician to test your hormones, which are all coming back relatively “normal”.
So, why are you experiencing symptoms? And more importantly, how can you stop them?
Hi friends. I’m Hilary Beckwith, ex-dieter and holistic nutrition expert. Clients come to see me with signs of adrenal stress and inflammatory conditions, and my job is to find the root causes so we can address their symptoms more effectively, and fill in the gaps between what their doctor is saying, and what their body is saying.
The adrenal glands do not get nearly enough limelight when it comes to addressing hormone imbalance symptoms. Dysfunction in the adrenal glands will disrupt hormone balance and cause issues with sleep, periods, mood, energy, and blood sugar levels.
Addressing adrenal health and stress management are the keys to getting better, more predictable periods, and improving mood and energy levels.
But there’s more to it than bubble baths or meditation.
In this article, you’ll learn:
how your body responds to stress
health effects of prolonged chronic stress
how to improve hormone imbalance symptoms by addressing chronic stress at the root
the body’s natural stress response
Stress is a normal part of human existence, and is modulated by the Autonomic Nervous System. It is necessary to keep us alive, and even become stronger!
Most stress is caused by what your brain perceives as a threat, but some stress is necessary for improving health, such as bone remodeling, building muscle, and cold plunging.
The stress your brain perceives as a threat (most stress), your body responds to as if it were a tiger. Evolution has not yet caught up to our modern lifestyles, and your brain cannot yet tell the difference between the threat of a tiger, and stress that comes from running late for a meeting.
When tigers are coming at you from all directions (work deadlines, heated conversations with your partner, toxic load from processed foods or medications, undiagnosed gut infections, people-pleasing behaviors, unaddressed emotional trauma, low blood sugar…), your stress response system will be constantly activated.
That chronic activation of the stress response system interferes with hormone production and balance. This is why effective stress management is essential to addressing hormone imbalance symptoms.
HERE’S HOW IT WORKS:
Is adrenal fatigue at the root of your insomnia and PCOS symptoms?
take the quiz
In response to a stressor, your fight or flight response is activated, and a feedback loop called the HPA axis (or hypothalamus, pituitary, adrenal axis) [1], stimulates your adrenal glands to produce stress hormones to increase energy production and increase blood flow to large muscle groups, heart, and lungs, to help you fight or flee the danger (tigers!).
When the threat has been successfully dealt with, the stress response stops, and your body returns to its rest and digest mode
If the stress becomes chronic, the system stays activated, and the adrenal glands adapt by producing less stress hormones, but more frequently.
TAKE A LOOK:
stressor or danger is sensed, and fight or flight response (a part of the Autonomic Nervous System) activates, signaling a cascade of events
the hypothalamus releases Corticotropin Releasing Hormone (CRH)
the increase in CRH signals the pituitary gland to produce AdrenoCorticoTropic Hormone (ACTH)
ACTH travels to the adrenal glands, signaling them to release stress hormones such as cortisol, adrenaline, and noradrenaline
these hormones begin the processes of energy metabolism (to fight or flee the stressor), and increase blood flow to large muscle groups, heart, and lungs
health effects of chronic cortisol release
The health effects of poor stress management impact more than just hormone imbalance symptoms. Chronic cortisol release has been shown to:
suppress the immune system [2]
cause sex hormone imbalance [3]
increase belly weight by way of insulin resistance [4]
increase inflammation [5] - Cortisol itself is anti-inflammatory, but its presence signals immune cells to react in response to stressors. This is inflammation. Chronic cortisol = chronic inflammation.
decrease thyroid hormone activity at a cellular level, causing elevated TSH levels on bloodwork
increase appetite by reducing leptin (hormone that tells you when you are full), and increasing ghrelin (hormone that tells you when you are hungry)
decrease digestive activity - when fight or flight is active, rest and digest cannot be.
causes poor sleep quality - the ability to fall asleep, stay asleep, and ultimately makes it difficult to get up in the morning.
Regarding hormone imbalance symptoms, the most important thing to remember about chronic stress is its ability to disrupt feedback systems for sex and reproductive hormones.
Take another look at the HPA axis. Components of this feedback system are also components of other important feedback systems, including the HPT (hypothalamus, pituitary, thyroid) axis, and the HPG (hypothalamus, pituitary, gonadal) axis.
When your fight or flight response is chronically activated due to poor stress management, or undiagnosed root-causes of stress, this will prevent hormone feedback systems from communicating properly, leading to hormone imbalance symptoms.
ways to improve stress management
I discuss methods for improving stress management at length in this article. But the best thing you can do for yourself right now, is to get data.
Let’s get curious about your symptoms and find out if there’s even anything to be concerned about.
want to dig deeper?
The REBALANCE Masterclass teaches you everything you need to know about supporting adrenal health.
was this helpful?
Please share your thoughts and questions in the comments below!
NUTRITION SERVICES
ADDITIONAL RESOURCES
BLOG REFERENCES
Slominski A. (2009). On the role of the corticotropin-releasing hormone signalling system in the aetiology of inflammatory skin disorders. The British journal of dermatology, 160(2), 229–232. https://doi.org/10.1111/j.1365-2133.2008.08958.
Segerstrom, S. C., & Miller, G. E. (2004). Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological bulletin, 130(4), 601–630. https://doi.org/10.1037/0033-2909.130.4.601
Ranabir, S., & Reetu, K. (2011). Stress and hormones. Indian journal of endocrinology and metabolism, 15(1), 18–22. https://doi.org/10.4103/2230-8210.77573
Kahn, Barbara B., and Jeffrey S. Flier. “Obesity and Insulin Resistance.” The Journal of Clinical Investigation, American Society for Clinical Investigation, 15 Aug. 2000, www.jci.org/articles/view/10842.
Hannibal, Kara E., and Mark D. Bishop. “Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation.” OUP Academic, Oxford University Press, 1 Dec. 2014, academic.oup.com/ptj/article/94/12/1816/2741907?login=false.